
What is irritable bowel syndrome?

Symptoms of irritable bowel syndrome

What causes irritable bowel syndrome?

Diagnosis of irritable bowel syndrome
Treatment of irritable bowel syndrome

Who treats irritable bowel syndrome?

Videos on irritable bowel syndrome
Monitor Bowel Symptoms
Additional resources
What is irritable bowel syndrome?
Back to topIrritable bowel syndrome, or IBS, is a functional gastrointestinal disorder or a disorder of the gut brain interaction in which patients experience chronic recurrent abdominal pain that is associated with altered bowel habits.
IBS is very common, affecting at least 6-11% of people by the new Rome IV criteria. But some studies estimate that less than half of people with IBS have received a formal diagnosis of this condition from a health care provider. IBS can occur in children as well as adults and seems to be somewhat more common in women than in men.
Symptoms of irritable bowel syndrome
Back to topSymptoms of IBS vary from person to person, and symptoms can fluctuate over time for the same person. There can be periods when symptoms flare up as well as periods when symptoms diminish or disappear. Some women experience worse symptoms prior to or during menstrual periods.
The most common symptom of IBS is chronic or recurrent abdominal pain. Pain is usually worse in the lower abdomen or pelvis but can occur anywhere in the abdomen. Abdominal pain is often associated with having a bowel movement, with a change in stool frequency, or with a change in stool appearance or consistency. For many people, pain improves after having a bowel movement, but some people have worse pain right after bowel movements.
Many people with IBS experience diarrhea, constipation, or alternating stool consistency. Women seem to be more likely to report constipation with IBS, but many women experience change in stool consistency, especially increased diarrhea, close to menstrual periods. Many people with diarrhea will note mucous in stools. Bothersome bloating is a very common symptoms in IBS, and tends to be worse in people who experience frequent constipation. Other common symptoms are urgency, or feeling that you need to have a bowel movement right away with very little warning, and the feeling of not completely emptying your bowels. Many people with IBS also report fatigue and difficulty sleeping.
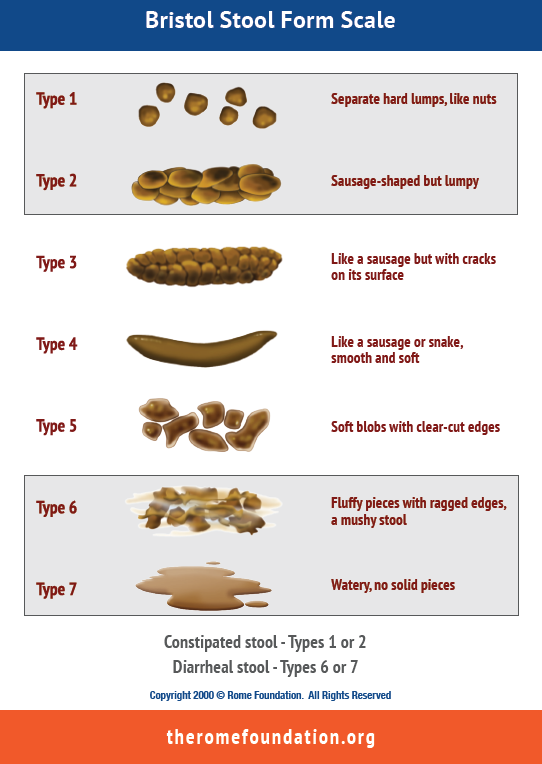
It can be difficult to know whether your stool consistency is “normal.” The only stool we usually see is our own, right?! The following figure contains visual images of various stool consistency classifications. Types 3-5 are considered normal consistency. It is common to have occasional constipation (firm stools, types 1-2) or diarrhea (loose stools, types 6-7). But it is not normal for the majority of stools to fall into constipation or diarrhea categories. It is important to note that a person can have constipation based on type 1-2 stools but still have a bowel movement every day.
What causes irritable bowel syndrome?
Back to topIBS is considered a “functional” condition, meaning that the intestines themselves appear normal on imaging studies, such as colonoscopy or CT scan, and histology, such as under a microscope. Rather, symptoms appear to be due to problems in the “function” or activity of the intestines, or in the regulatory mechanisms that control the GI system.
There seems to be a disturbance in the communication between the brain and gut, which is known as the “brain-gut axis.” There is not a consensus on the underlying cause of this altered brain-gut axis, but IBS likely results from combination of factors involving different mechanisms. Some of the mechanisms that may be involved in IBS include increased gut sensitivity (to foods or other stressors) and altered GI motility (meaning contractions of the bowel), altered immune function, gut microbiome (or bacteria in the gut), and central nervous system (meaning brain and spinal cord) processing of gut sensations.
Many people with IBS also have abnormal function in the pelvic floor muscles or muscles that support the rectum. These muscles play a very important role in stool continence, in other words, making sure that you have a bowel movement when it is desired or convenient rather that having a stool “accident.” As discussed in the Myofascial Pain module, these pelvic floor muscles can become overly contracted or tense and not relax as much as needed, which can place additional stress on intestines that are not functioning properly (called dyssynergic defecation).
Diagnosis of irritable bowel syndrome
Back to topCurrently there are no reliable laboratory tests, imaging studies, or other objective tests for diagnosing IBS. Often individuals with IBS will have seen many doctors before receiving a diagnosis of IBS because IBS can mimic other conditions, such as celiac disease and inflammatory bowel disease (or IBD). It is important to note however that you can have IBS in addition to having other medical conditions.
The diagnosis of IBS is based on symptoms. The key symptom of IBS is chronic or recurrent abdominal pain associated with altered bowel habits. The current criteria for diagnosis of IBS are the Rome IV criteria, which is a collection of the most common symptoms that typify this condition. This includes abdominal pain at least 1 day per week for three months that is associated with at least two of the following: 1) the pain is related to having a bowel movement, 2) the pain is associated with an increase or decrease in stool frequency, and/or 3) the pain is associated with the stools becoming harder or softer in form. The symptoms should have started at least 6 months ago.
There are also “supportive” symptoms, that are not technically part of the diagnostic criteria but are very frequently reported by people with IBS. These include abnormal stool frequency (> 3 bowel movements/day or < 3 bowel movements/week), abnormal stool form, excessive straining or urgency during defecation, feelings of incomplete evacuation, and mucus with bowel movements.
IBS is sub-grouped by predominant bowel habit. Because stool consistency is the best predictor of predominant bowel habit in IBS, stool consistency determines whether a person has IBS with predominantly diarrhea (IBS-D; >25% of bowel movements are loose or watery and < 25% are hard and lumpy), IBS with predominantly constipation (IBS-C; >25% are hard and lumpy and <25% are loose or watery), IBS with mixed bowel habit pattern (IBS-M; >25% loose or watery stools and >25% hard and lumpy), or IBS unclassified (IBS-U; <25% loose or watery stools and <25% hard and lumpy stools).
Your doctor should also look for signs and symptoms that are suggestive of conditions other than IBS, such as celiac disease or IBD (including Crohn’s disease or ulcerative colitis). They may recommend additional evaluation with a colonoscopy or other testing if you have not had age-appropriate colon cancer screening or if you have any of the following symptoms:
- gastrointestinal bleeding
- unexplained iron deficiency anemia
- unintentional weight loss
- palpable abdominal mass or significantly enlarged lymph nodes on exam
- family history of colon cancer
- onset of symptoms at age 50
- sudden or acute onset of new change in bowel habits should be evaluated clinically for other diagnoses even though IBS may be present.
Treatment of irritable bowel syndrome
Back to topTreatment of IBS does not have a one-size-fits-all approach, and will depend on the specific symptoms that a person is experiencing. For example, if you have IBS with chronic constipation, you will need different management strategies than someone with chronic diarrhea.
Because symptoms of IBS can be variable with time, it is common to experience symptom exacerbations even when you are using a very effective treatment regimen. Don’t be discouraged by these intermittent ups and downs, but do try to keep track of the general trajectory of symptoms. Some patients find that a symptom tracker or diary can be helpful to monitor the bigger picture of symptom control.
Self-Care
- Dietary modification - Several types of diets have been studied in people who have IBS or functional GI conditions. One of the most effective diets is called low FODMAP, which refers to specific foods that tend to be associated with more gas production. Other people find that symptoms worsen after they eat specific types of foods or beverages, such as caffeine, alcohol, fat, lactose, or gluten. As you can imagine, it may be very difficult to determine which types of foods are triggers for you. The goal is not to completely avoid all foods that have potential to cause issues, but rather to identify your specific trigger foods so that you can avoid these but otherwise eat a varied and satisfying diet. Some people find it helpful to see a specialized dietician who can help you navigate these “elimination” diets and properly evaluate your response. You can ask your health care provider for a referral to a specialized dietician.
- Physical activity - Several studies have shown that regular, mild to moderate intensity exercise can help reduce overall severity of IBS symptoms and may help reduce symptoms flares. See the Physical activity and exercise module for more details on what types of activities may be beneficial and how to begin an exercise routine in a way that doesn’t increase the chances of a symptom flare.
- Relaxation and Mindfulness – Did you know that there are more nerve fibers in your GI system than there are in your spinal cord? Intestines are covered with a thin web of nerve fibers which make up the “enteric nervous system”, and this system manages most of the normal day to day activity of the GI system. The enteric nervous system communicates with the central nervous system, specifically the sympathetic (“fight or flight”) and parasympathetic (“rest and digest”) parts of the central nervous system. This relationship may help you understand why you often experience GI sensations in response to emotional or psychological stress. Many people, even those without IBS, have had the experience of having diarrhea or constipation when going through a very emotionally stressful period, or having a terrible stomachache after receiving bad news. But abnormal activation of the enteric nervous system may be contributing to IBS symptoms in many cases. You may be able to influence the function of the enteric nervous system by increasing the parasympathetic activity of the central nervous system. Techniques introduced in the Relaxation and Mindfulness module increase parasympathetic activity, which may help reduce or manage IBS symptoms.
- Cognitive and Behavioral Strategies - Many people with IBS report significant stress or anxiety because of bowel symptoms or pain. It can be challenging to communicate with family or friends about the condition, particularly as stool consistency or frequency feels like a “private” issue. Techniques in the Cognitive and Behavioral Strategies module can help you manage the many ways that IBS affects your function and quality of life.
Professional Care
- Gastroenterologist or Primary Care Provider - You should work with a health care provider who has expertise in managing functional gastrointestinal conditions. There are also some medications or over the counter treatments that can be very helpful for many people with IBS, and your health care provider can make recommendations based on your symptom profile. As a reminder, a diagnosis of IBS does not mean that new or alarming symptoms should be ignored. Your health care provider can help you determine whether your symptoms warrant additional evaluation. You may request a referral to a provider who specializes in IBS or functional GI disorders if you do not feel that you are receiving adequate evaluation, education, or support.
- Specialized dietician – As discussed above, some of the dietary strategies to manage IBS involve eliminating and then reintroducing many different foods to determine your specific triggers. This process can be challenging to do alone, and a dietician who has experience managing IBS or functional gastrointestinal conditions may be extremely helpful. Many dieticians require a referral from your health care provider.
- Pelvic Physical Therapist – Pelvic myofascial pain is present in many people with IBS and can contribute to IBS symptoms like constipation or pain with bowel movements. Your health care provider can determine whether you have pelvic myofascial pain and provide a referral to a pelvic physical therapist if indicated. See Myofascial pain and Pelvic Physical Therapy for more details.
Who treats irritable bowel syndrome?
Back to topIBS is typically managed by a gastroenterologist or your primary care provider if they have training in this area. You may also benefit from consultation with a specialized dietician or pelvic physical therapist, depending on your specific symptoms and triggers.
Videos on irritable bowel syndrome
Back to topMonitor Bowel Symptoms
Back to topAdditional resources
Back to top[International Foundation for Gastrointestinal Disorders] (https://aboutibs.org/)

